One in Ten Americans Uses Painkillers

Not everyone who uses painkillers becomes addicted to them, but at least 33 million or more Americans are using addictive pain meds. The sheer prevalence of pain med use in America is more than a little bit shocking, especially given how dangerous these drugs are.
What is the scope of pain med use in the States? And why is it so critical that the use of these drugs be reigned in? It’s essential to look at how this came about, the risk factors involved in pain med use, and how pain prescribing should be FAR more conservative.
The Numbers – America is Addicted to Pain Meds
According to the Centers for Disease Control and Prevention, from 2015 to 2018, about 10 percent of Americans ages 20 and older used one or more prescription pain medications at least once in the 30 days leading up to the study. Almost six percent used opioid painkillers, and five percent used a non-opioid painkiller without a prescription.
That is a pretty shocking revelation that more than ten percent of the U.S. population experiences exposure to painkillers every month. It shows that the U.S. has become increasingly reliant on drugs to solve our problems, which carries a wide range of harmful repercussions.
“When taking into account that 21% to 29% of patients
prescribed opioids for chronic pain may misuse them, and 8% to 12% of these patients may develop opioid use disorder, the survey data showing greater than 1 of 20 U.S. adults using opioids for pain continues to be probletic...”
Dr. Yili Huang, director of the Pain Management Center at Northwell Health Phelps Hospital, commented on the findings, indicating what it means when almost 11 percent of Americans over the age of 20 are using pain meds. “When taking into account that 21% to 29% of patients prescribed opioids for chronic pain may misuse them, and 8% to 12% of these patients may develop opioid use disorder, the survey data showing greater than 1 of 20 U.S. adults using opioids for pain continues to be problematic. This stresses a need for continued pain management education as well as increased access to safe and effective pain care.”
At Risk—How Painkillers Often Do More Harm than Good
Opioid painkillers are addictive. Not even considering the mind-altering effects that one might get when he or she takes painkillers (mind-altering effects that one might become addicted to), merely the physiological nature of prescription pain relievers is addictive.
When opiate substances are put into the body, these chemicals react with opioid receptors in the brain. The result is that pain sensors are blocked from sending pain signals to the brain. However, the more one uses painkillers, the more the body comes to rely on these substances, even to the point where the individual will experience significant discomfort (withdrawal symptoms) if he goes for some time without taking painkillers).
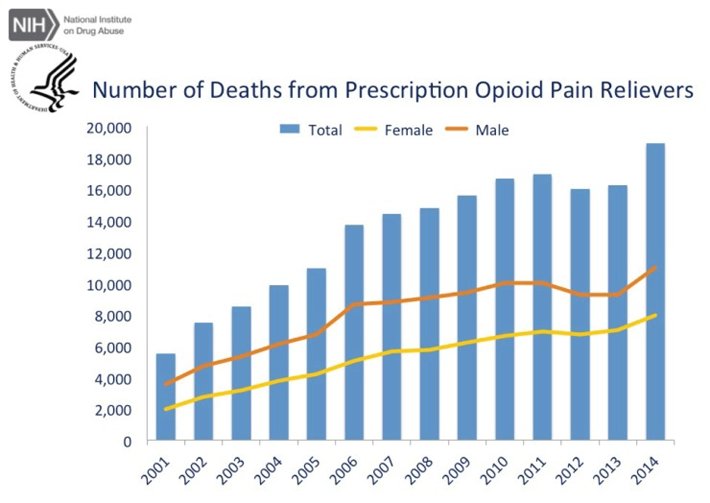
Another factor to consider is that the longer one uses painkillers and the more he uses, the more likely he is to overdose on them. Painkillers can be fatal and have killed tens of thousands of Americans since the turn of the century. That is why it is so essential to reduce prescribing trends across America, to make it so that far fewer than ten percent of American adults are taking these drugs.
CDC Prescribing Guidelines—There’s No Logical Reason Why One in Ten Americans Should be on Painkillers
Pain med prescribing should be far more conservative than it is. This is not a mystery. In the early-2000s, the medical community was widely “sold” this idea from pharmaceutical companies that OxyContin and other opioid painkillers were “nonaddictive.” That was a lie, and it is now more than obvious how dangerous these drugs are. While many prescribing physicians simply believed the pharma sales pitch and went along with it, many others were literally bribed by pharma companies to prescribe painkillers to patients.
To get doctors to curb their prescribing habits (which has been somewhat successful, though not nearly enough so), the Centers for Disease Control and Prevention released official prescribing guidelines. The full document is worth viewing, but we’ll take a brief look at points 1-12, below.
CDC Prescribing Guidelines:
- The CDC says that nonpharmacologic therapy and non-opioid pharmacologic therapy are, in fact, much preferred for treating chronic pain.
- Clinicians should establish realistic goals with patients, ensuring they understand the genuine risks in taking pain meds.
- Throughout treatment, clinicians should stay in touch with patients and ensure they do not take risks with pain meds.
- Clinicians should prescribe immediate-release pain meds when pain medication is necessary, not extended-release pain medication (such as OxyContin).
- Clinicians should prescribe the lowest effective dosage possible. Clinicians must understand that there is a risk in any dosage of pain medication.
- Opioid addiction often begins with the well-intentioned treatment of acute pain. Thus, clinicians should use the lowest effective dosage of immediate-release painkillers for the shortest duration possible to achieve a degree of pain relief for the patient. Three days or less is often sufficient.
- Clinicians must monitor patient success when pain meds are used for more than three days. This means regular and consistent follow-up.
- Clinicians should do everything they can to mitigate risk during the continuation of opioid therapy.
- Clinicians should always review each patient’s medical history before prescribing painkillers to pay special attention to any history of substance abuse.
- Clinicians should use urine testing before and during pain medication therapy, to ensure that they are not misusing, self-medicating, or taking other mind-altering drugs.
- Clinicians should avoid prescribing pain medication and benzodiazepines in tandem.
- Clinicians should offer a range of evidence-based treatments for patients who do become addicted to painkillers.
As one can likely imagine, many physicians do not follow all twelve of the CDC recommendations. This is a big mistake, as following these guidelines plays a prominent role in preventing addiction.
Drug Rehab—What to Do if You or a Loved One is Addicted to Painkillers
According to the American Association of Addiction Medicine, about two million Americans are addicted to prescription pain relievers. These individuals are at risk for a fatal overdose, which is why getting them help at a qualified drug and alcohol rehab center is so important. If you or someone you care about is addicted to pain meds, please contact Narconon today. Please do not wait until it is too late. Get help today and reverse the dwindling spiral of prescription painkiller addiction.
Sources:
- https://www.cdc.gov/nchs/products/databriefs/db369.htm
- https://www.usnews.com/news/health-news/articles/2020-06-24/1-in-10-americans-uses-a-prescription-painkiller-cdc
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6139931/
- https://www.cdc.gov/drugoverdose/pdf/prescribing/Guidelines_Factsheet-a.pdf
- https://www.asam.org/docs/default-source/advocacy/opioid-addiction-disease-facts-figures.pdf


